How To Fix Ozempic Butt In Menopause
Lost weight with GLP-1s, but have the dreaded "Ozempic Butt?" This article explains how to fix it.
Struggling with PCOS and weight that won’t budge? Here’s how GLP-1 medications are helping women at Josie.

The Josie Team
Medically Reviewed by

.jpg)
If you have Polycystic Ovary Syndrome (PCOS), you’ve probably been told to “just eat better and move more.” But what if your body doesn’t respond the way it used to… or the way it “should”?
For many women with PCOS, weight gain isn’t about willpower. It’s about insulin resistance, raging cravings, and a metabolism that’s stuck in storage mode.
That’s where GLP-1 medications come in. Originally designed for type 2 diabetes, they’re now helping women with PCOS feel more in control of hunger, cravings, and stubborn weight — even when nothing else has worked.
Most women with PCOS struggle to lose weight because the condition disrupts hormones that control hunger, fullness, blood sugar, and fat storage — making weight loss feel nearly impossible, even when you’re trying hard.
Here are the main reasons weight loss is harder with PCOS:
These challenges aren’t just frustrating — they’re biological. Let’s break down how PCOS impacts weight loss, starting with one of the biggest drivers: insulin resistance.
Most women with PCOS have some level of insulin resistance — even if they’re not prediabetic or diabetic. That means your body has a harder time using insulin to move glucose out of the blood and into your cells.
When insulin stays high, your body is more likely to store fat — especially around the belly.
And here’s the kicker: high insulin also drives cravings. So even if you’re eating “healthy,” your blood sugar may still be swinging wildly, triggering hunger that feels out of your control.
Melissa (35) has been a Josie patient for just over a year. She had spent over a decade trying every PCOS-friendly diet she could find. Low-carb, gluten-free, whole foods — she stuck with them all. And yet, nothing moved the scale more than a few pounds.
After a frustrating round of labs that again showed signs of insulin resistance, she told her provider, “I feel like my body just ignores everything I do.”
That’s when they started discussing additional support — including strength training, high-protein meals, and compounded GLP-1 medications designed for women like her.
With PCOS, your hunger and fullness hormones — like ghrelin (makes you hungry) and leptin (makes you feel full) — often don’t work the way they should. That means:
It’s not a willpower problem. It’s hormone chaos.
And trying harder — with more restriction, more cardio, and more guilt — can backfire, making the cycle even worse.
GLP-1s have shown to support the exact systems that are often disrupted in PCOS, including hunger cues, insulin response, and fat storage. They’re not a magic fix, but for many women, they make it possible to follow healthy habits without fighting their biology every step of the way.
Here’s how GLP-1s can help women with PCOS:
Now let’s look more closely at how these medications actually work.
GLP-1s slow digestion and increase satiety — meaning you feel fuller, longer. They also influence the hormones that regulate appetite, like ghrelin and leptin.
If you’ve ever felt like your body ignores fullness cues or your hunger “turns on” for no reason, this might be why. GLP-1s don’t erase cravings altogether, but they turn down the volume — so you're not fighting your body every day.
This isn’t a shortcut. It’s support.
Most women with PCOS have some degree of insulin resistance — even if they’re not prediabetic. That means their body struggles to process carbs effectively, leading to blood sugar swings and easier fat storage (usually around the belly).
GLP-1s like semaglutide and tirzepatide have been shown to improve insulin sensitivity and reduce fasting glucose levels in women with PCOS. For many, that means breaking the frustrating “storage mode” cycle.
Melissa’s labs kept showing insulin resistance despite years of clean eating. Once she started GLP-1 treatment through Josie, her provider tracked improvements not just on the scale — but in her fasting glucose and energy levels too.
For women with PCOS, sometimes food and movement aren’t enough. You may need tools, like GLP-1 therapy, that meet your biology.
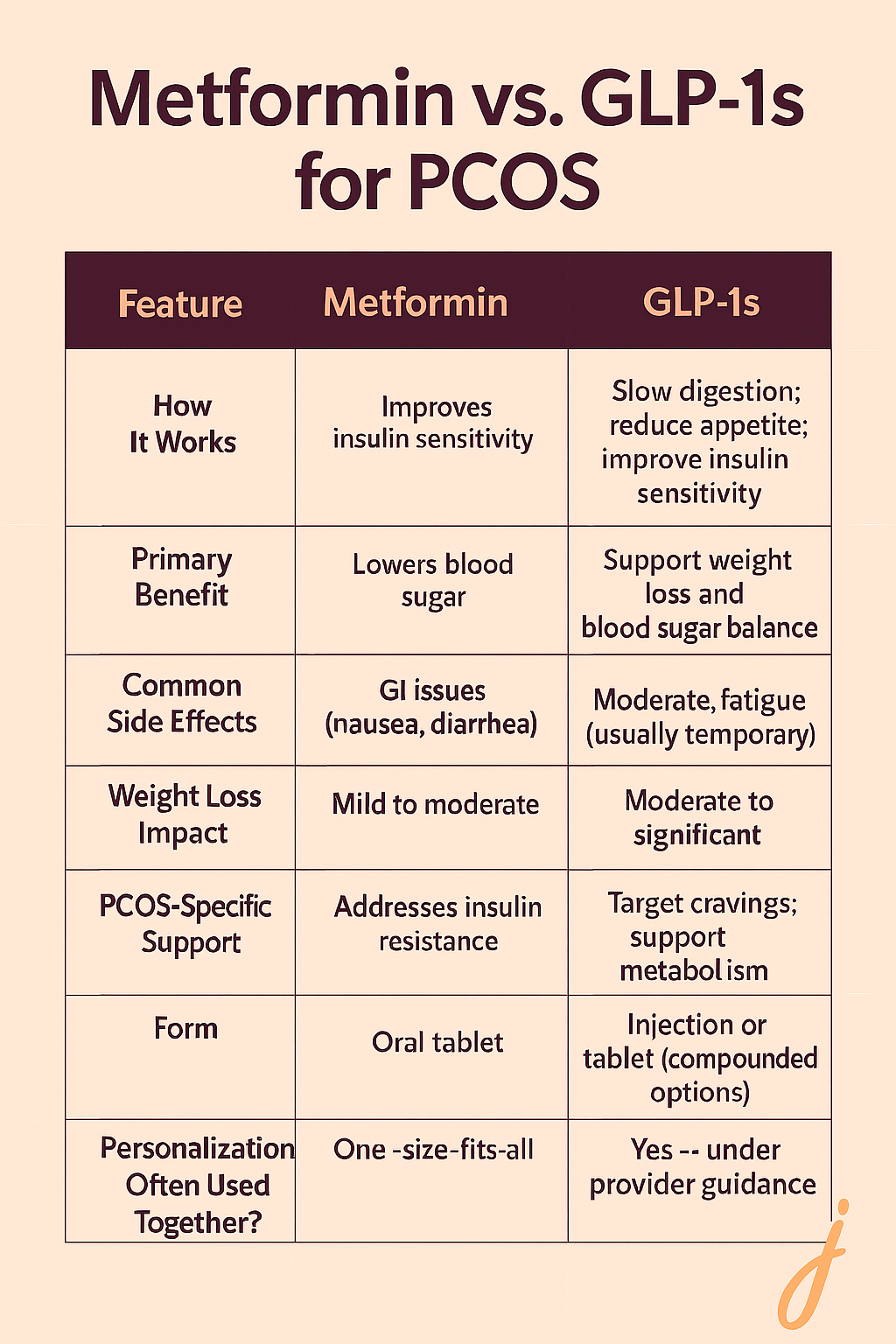
The truth is, they work in different ways. Metformin helps improve insulin sensitivity at the cellular level. GLP-1s go a step further by targeting appetite, cravings, and multiple metabolic pathways.
Some women use both together, while others move from metformin to GLP-1s when metformin alone isn’t enough.
If metformin helped a little but not enough — or caused side effects — a GLP-1 may be a better next step.
For many women with PCOS, the hardest part isn’t just the weight — it’s feeling like you’ve lost control of your body.
At Josie, we hear it every day:
“I was eating clean and exercising. Nothing changed. I thought it was me.”
But once those women started GLP-1 therapy tailored for PCOS, things began to shift.
Melissa is one of many. But she’s not the only one.
Across Josie, we see a pattern:
GLP-1s aren’t a magic fix. But for women with PCOS, they offer something better: a biology-based tool that works with your body, not against it.
Jenna (35), another Josie patient, had lived with PCOS since her early 20s. Her symptoms weren’t just physical — they were emotional. Constant fatigue, relentless cravings, and a scale that never moved no matter how “perfect” her eating was.
“It felt like I had to outsmart my body just to maintain my weight,” she said. “And losing any? Forget it.”
After yet another restrictive diet that led nowhere, Jenna found Josie. Her provider listened closely, reviewed her labs, and explained that PCOS-related insulin resistance was likely at the root of her struggles. Together, they decided to start compounded GLP-1 therapy.
But that wasn’t all. Josie also recommended strength training — something Jenna had never done in her life. With a little hesitation, she signed up for the Simply Strong App (programmed strength training workouts for women 35+). “They made it so approachable,” she said. “Workouts were quick, and I actually felt strong by week two.”
She also began using the 500+ high-protein recipes in the app to rebuild her meals in a way that worked with the medication.
Three months in, the difference was night and day.
“My cravings finally quieted down. I wasn’t constantly exhausted. And I felt like I had a plan that was working for my body, not against it.”
Jenna didn’t just lose inches. She gained confidence, consistency, and a sense of control she hadn’t felt in over a decade.
Yes, both brand-name and compounded GLP-1 medications can be safe for women with PCOS, even without type 2 diabetes. While these meds were originally developed for blood sugar control and diabetes management, providers now often use them off-label to help with PCOS-related weight challenges — especially when insulin resistance is a factor.
Clinical studies show that GLP-1 medications (like semaglutide and tirzepatide) improve insulin sensitivity, reduce inflammation, and support weight loss in women — even those without diabetes. This makes them a helpful tool for managing one of PCOS’s toughest symptoms: stubborn weight gain.
Compounded GLP-1s are custom-formulated by licensed compounding pharmacies and prescribed under medical supervision. At Josie, every prescription is reviewed by a licensed U.S. provider who monitors your labs, symptoms, and progress — making sure it’s the right fit for your body and goals.
Like all medications, GLP-1s can come with side effects — most of which are short-term and manageable when dosed properly. These include:
Josie’s providers use a slow titration schedule to minimize side effects and personalize your care. You’ll also have 24/7 messaging access to check in if anything feels off.
While most women experience only mild or temporary side effects, there are rare but more serious risks to be aware of — especially if you have a personal or family history of certain medical conditions. These include:
Important: GLP-1 medications — including compounded versions — are not recommended for anyone with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2).
At Josie, your provider will screen for these risk factors before prescribing. And if anything changes during treatment, you can always reach out through the app to adjust your plan safely.
GLP-1 medications can be a powerful tool — but they’re not magic on their own. To get the best results and support your body long-term with PCOS, you’ll still need to build a foundation with food, movement, and rest.
That includes:
Protein helps you feel full, stabilize energy, and support lean muscle — all things that make your GLP-1 work better. It also helps reduce the blood sugar spikes and crashes that worsen PCOS symptoms.
Some PCOS-friendly food habits to try:
Muscle isn’t just about looking toned — it’s your metabolism’s best friend.
For women with PCOS, strength training improves:
Even beginners see results fast. Josie patients often start small — just two workouts a week — and build from there. We highly recommend the Simply Strong App.
PCOS symptoms get worse when your body is under stress. Cortisol — your stress hormone — can increase belly fat storage and make insulin resistance harder to reverse.
That means:
Josie’s providers talk with patients about more than medication — they offer realistic, judgment-free guidance around the stressors midlife women face every day.
If you’ve been told to just “try harder” or “eat less, move more,” you’re not alone — and you’re not doing anything wrong.
PCOS disrupts the very systems that regulate hunger, blood sugar, and fat storage. It’s not a lack of willpower. It’s biology.
At Josie, we see women every day who’ve done everything right and still struggle. GLP-1 medications — especially when paired with strength training and high-protein meals — have helped them finally feel in control again.
You don’t have to keep fighting your body. There’s support that works with it.
Can GLP-1s help me lose weight if I have PCOS but not diabetes?
Yes. Many women with PCOS use GLP-1s off-label to support weight loss. These medications help regulate appetite, reduce cravings, and improve insulin resistance — all common struggles in PCOS. At Josie, a licensed provider reviews your history to ensure it’s a safe fit.
What’s the difference between Metformin and GLP-1s for PCOS?
Metformin may improve insulin sensitivity, but doesn’t target appetite. GLP-1s do both. Some women use one or the other, and some combine them. Your provider can help decide what’s best based on your symptoms and goals.
Are compounded GLP-1s safe?
When prescribed through a licensed provider and filled at a certified 503A pharmacy, compounded GLP-1s can be a safe and effective alternative to brand-name meds — especially when cost or availability is an issue. Every Josie prescription is reviewed for safety and appropriateness.
Do I need to be doing everything “perfect” for GLP-1s to work?
No, but the meds work better when paired with high-protein meals, strength training, and stress management. You don’t have to be perfect. You just need the right tools and support to stay consistent. That’s why Josie pairs every plan with resources and check-ins.
How long does it take to see results?
Many women start noticing reduced cravings and better energy in the first few weeks. Weight loss may begin more gradually, depending on your dose, habits, and hormones. Sustainable results take time — and consistency pays off.
Take our quick quiz to see if you're a candidate for compounded GLP-1 support through Josie.
We'll personalize your plan, walk you through your options, and connect you with a licensed provider who understands PCOS.
Take the 2-minute quiz!