How To Fix Ozempic Butt In Menopause
Lost weight with GLP-1s, but have the dreaded "Ozempic Butt?" This article explains how to fix it.
This guide helps women in menopause learn about GLP-1 weight loss.

The Josie Team
Medically Reviewed by


GLP-1 medications are prescription treatments that support weight loss by helping regulate appetite, blood sugar, and fullness signals. Women in perimenopause and menopause are becoming a large percentage of GLP-1 users because hormonal changes often make weight management more difficult than it used to be.
Understanding GLP-1 therapy during midlife can feel overwhelming. Every provider takes a different approach. Dosing methods vary. Some programs are designed for women with hormonal changes and others are not. At the same time, there is strong interest in finding safe, sustainable weight loss support during menopause without unrealistic promises.
In this guide, we take a closer look at how GLP-1 medications fit into midlife weight management, the factors that matter for women with hormonal changes, and the key differences between programs so readers feel informed and confident in their decision.
Weight loss during midlife is not just about lifestyle. It is influenced by biological shifts that change how the body manages fat storage, hunger, and energy. These changes affect metabolism, muscle mass, and blood sugar response, which can make weight loss feel harder than it used to.
Several factors contribute, including:
These changes create a situation where women can eat well, exercise, and still struggle with weight gain or stalled progress. GLP-1 medications do not reverse menopause, but they work with these biological processes to help appetite and blood sugar become easier to manage.
Next logical question:
If biology changes, how do GLP-1 medications fit in?
GLP-1 medications mimic a hormone the body already makes to manage appetite and blood sugar. During menopause, these two systems become more sensitive and less predictable, which is why hunger, cravings, and energy can feel different than they used to. GLP-1s help bring those signals back into balance so weight loss feels more manageable instead of like a constant battle.
Here is what is happening inside the body:
Women often describe the first noticeable difference as a mental shift. Food stops taking up so much space in their thoughts. They are not fighting hunger or trying to distract themselves from cravings. They still eat, but the sense of urgency around food settles.
When hunger is manageable, it becomes easier to:
These effects are especially supportive in menopause because hormonal changes can cause:
GLP-1 medications do not replace healthy habits, and they do not guarantee results on their own. They create the space for habits to work by turning down the biological resistance that often appears during midlife. Women see the best outcomes when hunger is calm and nutrition and strength training are part of the routine.
Learn how GLP-1 medications change a woman’s body.
Next, we'll discuss potential results and what to expect.
Results vary from woman to woman, but there are consistent patterns in how progress unfolds during midlife. The body responds in stages rather than all at once.
The first changes are usually non-scale wins, often within the first few weeks:
These changes matter because they set the foundation for weight loss that does not rebound later.
Visible changes often follow next. Women may notice:
Not everyone loses weight at the same pace. Women who pair nutrition and movement with the medication tend to see the most steady and comfortable progression. Discover more non-scale progress markers women experience on GLP-1s.
Weight loss timelines vary, but these general patterns are common among midlife users:
The goal is not to rush the process. The goal is to give the body enough time to adjust so progress feels smooth and sustainable rather than extreme.
Seeing progress leads to the next question women commonly have… “how long should I use it for?”
There is no single correct timeline. The right length depends on your goals, your metabolism, and how your body responds during the process. What matters most during menopause is not getting off the medication fast, but allowing enough time for your appetite, eating patterns, and energy to feel steady and reliable.
Many women start with the idea that shorter is better. With time, most realize that support during the transition is what protects their progress, not rushing to finish as quickly as possible.
Here is how GLP-1 timelines commonly unfold during midlife:
Staying longer is not a failure. Stopping sooner is not a badge of honor. Menopause changes the rules, which means every woman deserves a timeline that supports her biology instead of fighting it.
There are also moments when women naturally reassess their plan:
Some women continue the medication for weight maintenance. Others taper slowly. Others take breaks and come back later. There is no wrong path as long as your decision is based on how your body feels rather than pressure or guilt. Learn more on what the usual duration looks like for menopause users.
And that realization leads to the next question almost every woman asks once she feels more in control of her hunger:
If the medication quiets cravings, what should I be doing to shape my body and protect my metabolism while I am on it?
That question matters because GLP-1s make weight loss easier, but they do not decide how your body looks or feels after the weight comes off.
GLP-1 medications lower hunger. That creates space to build habits that shape how your body looks and feels during and after weight loss. Women in menopause see the most confident and long-lasting results when the focus is not just losing weight, but supporting muscle, metabolism, and recovery at the same time.
The most important habit during this time is strength training. It replaces the muscle that is normally lost during menopause and weight loss. More muscle means a faster metabolism, better shape, and a higher likelihood of keeping the weight off.
For women on GLP-1s, a simple structure works best:
When the program is designed well, each day targets different muscle groups and includes the areas women care about most: glutes, thighs, arms, shoulders, back, and core. That is why women in the Josie community often use the Simply Strong App. It was created by a woman in midlife for women in midlife, and the workouts follow progressive overload without burnout. Women tell us that the structure makes it easier to stay consistent even on busy weeks because they do not have to guess what to train.
Nutrition supports muscle and energy during this process. The most reliable and easy rule is:
Eat your goal weight in grams of protein per day.
Example: If a woman wants to weigh 130 pounds, she aims for 130 grams of protein per day.
Eating enough protein helps:
Hydration, fiber, and balanced meals help digestion adjust comfortably, but protein is the most important for body composition.
Sleep is another factor that matters more during menopause. Muscles are not built in the gym. They are built during rest. Poor sleep makes cravings stronger and recovery slower. Even one or two nights per week of deeper sleep can noticeably improve strength and energy.
Gentle daily movement such as walking supports circulation and recovery. It is not required for weight loss, but it helps women feel better while their bodies adjust.
None of this has to be perfect. Women do not need strict macros or two hour workouts. The combination of strength training, protein, sleep, and light movement is powerful because it works with the medication, not against it. See how women at Josie shift from weight loss to muscle-focused on GLP-1s.
When these habits are in place, you’ll start to focus on maintaining your results in the long run so you don’t regain the weight and progress you’ve made.
Women who keep their results long term do not succeed because they never slip. They succeed because they build a routine that naturally supports their goals even when motivation changes. The most predictable path to lasting results is not trying to control every meal or every craving. It is building environmental stability around the habits that were working during the medication phase.
Instead of focusing on what to do, maintenance focuses on how to stay consistent with the habits that worked before.
Women who maintain their progress typically rely on four stability anchors:
1. A weekly rhythm instead of daily pressure
Planning workouts and meals by the week instead of day by day removes guilt and decision fatigue. Consistency becomes flexible, not rigid.
2. A backup plan for lower motivation days
A short home workout, a protein shake lunch, or an early bedtime serves as a “minimum effective fallback” when life gets busy. Having a backup plan prevents reverting to old patterns.
3. Tracking how the body feels rather than only the scale
Energy, strength, digestion, sleep, and confidence often provide earlier and more accurate signals than weight. Women who focus on these indicators adjust faster and avoid spirals.
4. Automatic cues built into the environment
Small but powerful examples include:
Maintenance is not about being perfect. It is about staying in a rhythm where habits require less effort to follow than to abandon.
If you think GLP-1 therapy could be a fit, how should you choose a provider that actually supports women in menopause?
Not all GLP-1 programs are the same. Many were designed for general weight loss and do not take hormonal changes into account. Women in perimenopause and menopause often need a different level of personalization because appetite, muscle, digestion, stress response, and sleep all influence weight differently during this stage of life.
The best provider is the one that makes weight loss feel manageable and sustainable for a midlife body. Women usually feel the biggest difference when the program supports their biology instead of treating them like younger patients with different needs.
Here are the factors that matter most when choosing a provider in menopause:
1. Dosing designed for hormonal sensitivity
Midlife women often respond better to gentler dose increases, especially during the first few months. Programs that follow a one-size-fits-all schedule can create preventable side effects that lead to frustration or dropout.
2. Support when symptoms fluctuate
Hormone-related appetite shifts, stress, and sleep changes can affect how GLP-1s feel week to week. Providers who offer check-ins and clear communication tend to help women stay consistent without guessing.
3. Nutrition and protein guidance
Women who protect muscle while losing weight maintain better shape, energy, and metabolism. A provider that supports protein intake and strength training helps protect results long term.
4. Access without barriers
Long wait times, limited deliveries, or complicated insurance steps can make it difficult to stay on track. Consistency is easier when the program is simple and reliable.
5. Flexible pathways, not pressure
Women do best when they can shift between microdosing, full dose, oral options, or taper plans based on how their body feels, instead of being locked into one approach.
Many GLP-1 providers do not meet these criteria because their systems were built for general weight loss rather than hormonal complexity. When a program does take menopause into account, women typically report smoother progress, fewer side effects, and a stronger sense of control.
At Josie, these principles shaped the program for a reason. The dosing approach is gradual. Support is continuous. Nutrition and strength training are part of the model because they protect muscle and metabolism in midlife. And women can choose microdose, standard dose, oral options, or taper plans based on how they respond rather than how the software dictates.
Many women compare Josie vs Hers, both great GLP-1 programs for women in menopause.
Once a woman finds a provider that understands hormonal changes, the next decision is usually which medication to choose
Semaglutide or tirzepatide?
Semaglutide is often the better fit for women who want a gentler and more gradual appetite change, while tirzepatide may be the better fit for women who want a stronger appetite reduction and faster results. Both support weight loss in menopause, but they feel different in the body.
Semaglutide is a GLP-1 agonist.
It mimics the natural hormone GLP-1 to support appetite regulation, blood sugar balance, and fullness signals. Many women describe it as smooth and steady.
Tirzepatide is a GLP-1 + GIP dual-action agonist.
Along with GLP-1 activity, it also activates GIP receptors, which can create a stronger effect on appetite and insulin response. Many women describe it as faster and more powerful.
Take a look at the graphic below to see the main differences:
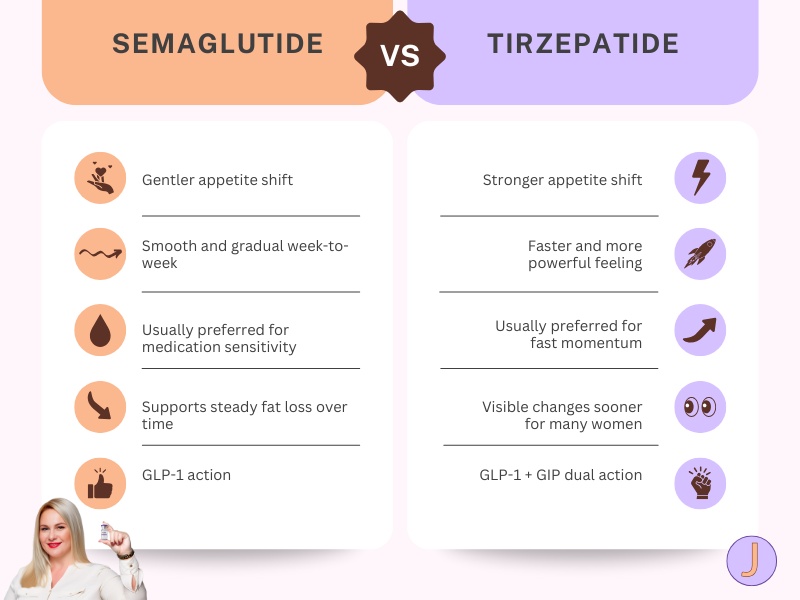
Find out how dual-action GLP-1 + GIP compares with single-action GLP-1 in menopause.
Both compounded and brand-name GLP-1 medications support appetite regulation and fullness. The difference is not which one is better, but which one aligns with a woman’s medical needs, preferences, and access options.
Brand-name options
Other brand-name GLP-1 medications commonly used clinically
Women may choose brand-name GLP-1s if they want:
Women may choose compounded GLP-1s (usually added with vitamin B6 or B12) if they:
Some women feel compounded GLP-1s appear to be more affordable, especially when paying out of pocket. That may shift in the future as programs like TrumpRx aim to make brand-name medications more accessible, so affordability is not a static factor.
At the end of the day, a woman is not choosing the “right” or “wrong” category. She is choosing the model of care and access that makes her feel supported, safe, and successful long term.
Learn more about compounded GLP-1s vs Brand Name GLP-1s.
What about dose? There’s microdosing, or full therapeutic dose, but what’s the right choice? We’ll cover that next.
Microdosing is often the better fit for women who want a gentle introduction to GLP-1s with minimal side effects, while a full therapeutic dose may be better for women who want faster appetite reduction and are comfortable increasing dosage more quickly.
Women who choose microdosing usually want:
Women who choose a full therapeutic dose usually want:
Both paths can be effective during menopause, and neither is “better.”
The choice is about comfort level and sensitivity, not willpower or motivation.
Learn more: microdosing GLP-1s vs full therapeutic dosing
If you’re unsure where you fit, it can help to think about how your body typically responds to medication and hormone changes. Some women need a gentler start. Some want powerful momentum. Both choices are valid.
What about delivery? There are oral options and injections, and they feel different in the body. We’ll break that down next.
Injectables are often the better fit for women who want the most consistent and predictable GLP-1 absorption, while oral GLP-1s may be the better fit for women who prefer not to use needles and want a more gradual appetite shift.
Women who choose injectables usually want:
Women who choose oral GLP-1s usually want:
Both forms support weight loss in menopause.
The difference is dose style and comfort, not “strength” or “discipline.”
Learn more: Oral GLP-1 vs Injectable GLP-1
If you’re still unsure, the next question many women ask is about side effects, not because they’re guaranteed, but because what you do in the first few weeks can make a big difference in comfort.
Let’s break down side effects for women with hormonal changes and how to minimize them.
In our experience supporting midlife women on GLP-1s, responses vary widely. Some women feel a smooth transition, while others need time, slower titration, or dose adjustments to feel their best. Neither experience is a sign of success or failure. It simply reflects how each body responds to hormonal and metabolic change.
The most common effects menopausal women on GLP-1s notice in the first few weeks can include:
These typically happen because appetite signals begin to shift and digestion slows.
You can reduce discomfort by:
The most important thing is communication. You do not need to push through discomfort. Staying in contact with your Nurse Practitioner or Doctor allows them to personalize your plan with the right dose timing, titration speed, and nutrition guidance so your body can adjust comfortably.
Side effects are not a sign that GLP-1s are not working. They are simply a sign that your system is adapting. With support, you could feel noticeably better over time.
So how do you get started safely? And what does getting started look like?
The safest way to start a GLP-1 is with support from a provider who understands the hormonal and metabolic changes of midlife. GLP-1s work best when the dose, form, and titration schedule match your sensitivity, eating patterns, and energy levels rather than a one-size-fits-all plan.
Here is what the starting process usually includes:
A good program will also explain:
Women feel the most confident when:
GLP-1s are not about perfection. They are about giving your body room to respond and finding a rhythm that lets weight loss feel achievable instead of exhausting.
GLP-1 therapy during menopause is not about perfection or doing everything at once. It is about lowering the friction around hunger and creating the space for routines that support your metabolism, strength, and confidence. When progress feels steady instead of forced, it becomes easier to stay consistent and trust the process.
Every woman’s journey looks different. The right path is the one that works with your biology, feels sustainable for your lifestyle, and allows you to feel like yourself while you make progress. If your hunger is calmer and your routines feel easier, you are moving in the right direction.